An update from our Chief Medical Officer:
I have read more lately about the current state of summer doldrums and pandemic fatigue, and I can definitely relate. We are all anxious for schools to open, business to thrive, sports to resume play, movie theaters to distract us, and friends and family to visit us.
- “No question, epidemic fatigue or pandemic fatigue is real. We are experiencing it,” Markel said. “But throughout human history, there have been terrible pandemics and contagious threats. Every civilization, every nation, has come through to the other side. And we will, too.” Washington Post, 8.11.20
But, I am also very accustomed to the new norm of mask-wearing, limited travel, physical distancing and hand and cough hygiene. As always, I encourage you all to help support each other during the down times and to remain optimistic and hopeful. Refer to our Employee Assistance Program, the HealthJoy app or speak with a colleague or supervisor. There is a lot to be encouraged by, despite the ongoing situation.
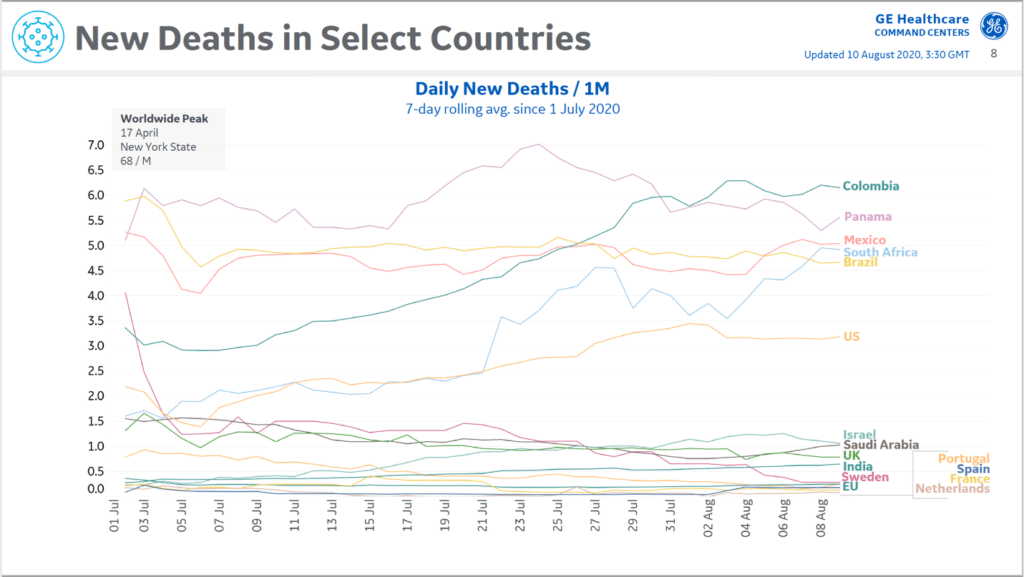
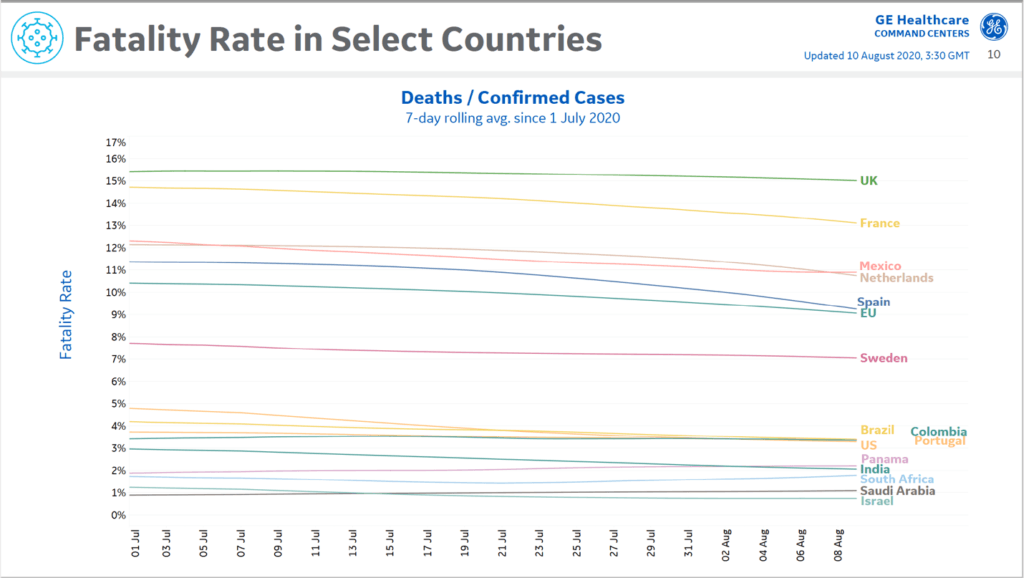
The universal mask-wearing recommendations from the highest levels of government and health officials seems to be having the intended effect. New case counts in the US have overall stabilized and decreased since our last update and even the death counts that inevitably trail the acute cases and hospitalizations is slightly improved from last week’s peak, except in a few remaining hot spots. And our mortality rate in the US is lower than Europe, likely due to the recent surges being concentrated in children and young adults who generally have better outcomes. We also have some new and better treatments for severe cases.

• New cases continue to drop significantly in the Southeast and Southwest. Slight uptick in cases in the Midwest. New cases in Northeast remain low.
• Inpatient COVID-19 hospitalizations have remained relatively stable in the last couple of weeks.
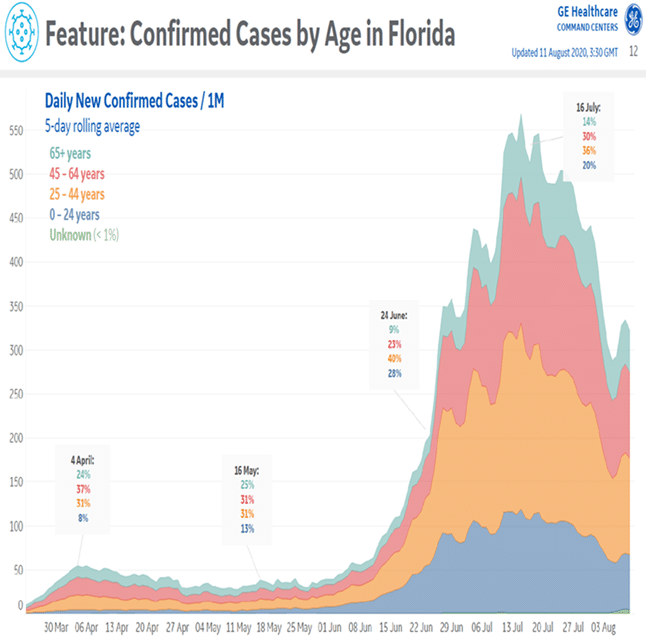
• The majority of new cases in FL are in the population less than 44 years old (56%), while hospitalizations are in those greater than 44 years old (83%). This is similar data in Florida as compared with a month ago.

There remains much continued debate and new evidence emerging weekly regarding masks and PPE that I would like to address. Many of you may have seen a recent study from Duke that reports neck gaiters prove very ineffective as a ‘cloth face covering’ for coronavirus and potentially are even worse than no mask at all. So please wear a true ‘face mask’ and avoid close contact situations like elevators or retail/grocery stores that place you in direct contact with a gaiter-wearing patron.
Study: Masks of almost any type may slow, stop coronavirus spread
- The Hill (8/11, Weixel) reports, “A new study adds to the growing evidence that masks (not gaiters) of almost any type will help slow and stop the spread of the coronavirus.” The researchers “found that most types of homemade masks are better at preventing the spread of droplets than nothing at all, but the effectiveness largely depends on their material and fit.” Their findings were published in Science Advances.
As indicated from the beginning, science is driving our decisions and as data is expanded, clarified and updated, we continue to modify our policies and protocols. Even Dr Fauci originally discouraged widespread surgical face mask use due to the fear of public consumption, stock-piling and price gouging to the detriment of front-line health care workers, especially when the primary mode of transmission was thought to be ‘fomite’ or surface contact between coronavirus and nose, mouth and eyes. The CDC originally only recommended face masks for symptomatic patients. But then evidence emerged about asymptomatic and pre-symptomatic community spread and simultaneously home-made and manufactured non-medical cloth face coverings were determined to be very effective for both source control and personal protection. The CDC updated its guidance appropriately. A recent analysis published by Goldman Sachs Research suggests that expanding community masking by 15% could prevent the need to bring back stay-at-home orders that would otherwise cost an estimated 5% of gross domestic product, or a projected cost of $1 trillion. “So, just wear a mask!”
And this applies to all areas of the QDP office setting, breakrooms, work-stations and clinical space so that employee exposure and prolonged quarantines are avoided.
- “At this critical juncture when COVID-19 is resurging, broad adoption of cloth face coverings is a civic duty, a small sacrifice reliant on a highly effective low-tech solution that can help turn the tide favorably.” JAMA 7.14.20 Brooks JT et al. CDC Directors
Early on we issued guidance on more liberal N95 use which has since been updated in our OSHA policy after extensive literature review and counsel by multiple sources. The aerosolization risk posed by our various dermatologic surgical procedures is not well quantified, but is definitely now considered low, relative to the known high-risk aerosol-generating procedures like intubation, bronchoscopy, oral surgery, etc. Our patients by definition have been thoroughly screened and overall pose a low risk, especially being masked. We have balanced our approach using professional society recommendations for responsible use of PPE understanding that front-line health care workers have a great need for this equipment, which frustratingly still remains in short supply nationwide. We continue to explore every avenue for acquiring PPE in various sizes and types.
Strategies to re-sterilize N95s include the previously referenced brown bag storage x 3 days; microwave steam protocol; and a new one published this week in JAAD that relies upon dry heat (see below). Another study this week in JAMA further confirms the overall low risk of C-19 transmission in health care workers even with standard surgical masks in high risk settings and expounds upon alternative options for added protection. These options include KN95 masks; adding a plastic face shield to standard surgical masks; adding a standard surgical tie-back mask over an N95 to improve the side seal (tie-back masks afford double the lateral seal protection compared to ear loop masks). Smoke evacuation systems can also be used during laser and electrosurgery for high risk anatomic sites (mouth/nose) and are being made available.
Proposed approach for reusing surgical masks in COVID-19 pandemic. JAAD July 2020 E53.
- Heating at 150 – 160oF can be achieved by baking in an oven, incubator, or even a blanket warmer for 30 minutes without reduction in filtration efficiency after 20 cycles. […this method provides a simple, straightforward, and effective strategy for decontamination of used masks.]
Finally, an editorial in JAMA supports our personal experience at QDP of low risk for HCP in that all known QualDerm employee coronavirus exposures and/or infections have occurred in the household, community or non-clinical setting with none traced to a known or suspected occupational clinic exposure. We remain extremely vigilant and committed to ensuring high safety standards for all our valued staff and trusting patients and continue to constantly reevaluate our strategies. You are truly our greatest asset.
Another issue arising lately relates to the screening and triage protocol. I know a few sites are piloting the smell test reviewed last month and I’ll be interested in their impressions. Loss of smell and taste remain among the most highly specific symptom of COVID-19 so some degree of testing is reasonable, although not required. Some clinics have also recently questioned the necessity for capturing screening questions at both the front desk and later in the dermatology exam room. Our cautious rationale has been to utilize the front desk to eliminate obviously sick patients from potentially infecting the waiting room or other personnel prior to their visit, according to CDC guidance. The clinical staff can then perform a rapid repeat screen to verify accuracy and document the triage protocol in the medical record, including any qualifiers such as a known diagnosis being evaluated and/or under treatment by another clinician. Our IT staff has added a free text box to the EMR to allow documentation if, for example: smelling loss started 10 years earlier (true case); a headache was known to be a typical migraine; or diarrhea due to known food poisoning. We would not necessarily expect a non-clinical and very busy front desk receptionist to capture and document this information as well as clinical nursing staff so the redundancy is by design, a double check.
Other news and developments in the COVID-19 landscape:
- Russia’s announcement of a new vaccine is likely a political tactic rather than a scientifically valid development, given that no Phase 3 placebo-controlled randomized trials have been undertaken yet to confirm either its safety or effectiveness
- US trials are much further along in testing and manufacturing for numerous candidate vaccines, with hopes for adequate doses by early 2021 of multiple effective agents that can target diverse populations and improve outcomes for different patient severities
- In a rare agreement between drug companies, Pfizer said it would help manufacture remdesivir, made by Gilead Sciences, to increase the supply of the drug, which some hospitals have had to ration among Covid-19 patients.
- Convalescent Plasma Could Reduce Death From COVID-19, Early Data Suggests. (LiveScience) –COVID-19 patients treated with the blood of those who have recovered from the infection die at significantly lower rates than those given standard treatments alone, according to a preliminary analysis.
- Inspired by a unique kind of infection-fighting antibody found in llamas, alpacas, and other camelids, a research team at the University of California, San Francisco, has synthesized a molecule that they say is among the most potent anti-coronavirus compounds tested in a lab to date.
- Public transportation may not be a major source of coronavirus transmission, studies suggest. A lot remains unknown, but the Times reports that riding public transportation probably falls somewhere in between walking outdoors and dining indoors on the safety scale.
- Given ongoing inadequacy and delays in COVID-19 testing, the AMA and other organizations sent a letter to Health and Human Services Secretary Alex Azar asking “the administration to update the testing guidelines to prioritize those with a medically-indicated need for a COVID-19 test, including those with symptoms of the virus, those with known exposure and those in need of pre-procedure testing.”
Please continue to provide suggestions or ideas so we can address questions or concerns. Have a good and safe weekend!
Sincerely,
John Albertini, MD