Provider Pulse - December 2025
 Dear Colleagues:
Dear Colleagues: As we wrap up the year, I want to take a moment to reflect on key areas that we have improved this year, areas of continued improvement, and anticipated areas of focus in the new year.
Firstly, on the clinical side, quality patient care remains our anchor. Across the QualDerm network, our clinical performance has stayed strong. We have improved patient access through online booking options and triage models in many markets—initiatives that continue to expand. Patient reviews have been predominantly positive, and we have continued to enhance providers’ experience. I recognize there are still opportunities to improve quality, and I look forward to launching a new quality improvement program next year.
On the compliance side, we have done well with CLIA, MIPS, and participation in our Compass Coding program. Still, documentation accuracy and visit-level complexity coding continue to show avoidable variation. These are correctable issues and getting it right matters - not only to ensure that revenue accurately reflects the services provided, but also for the integrity of the clinical record and the downstream care our patients receive. To improve our documentation and coding, I am working on specific training on this topic for all our providers, coming in early 2026.
Thank you for the work you have put in this year. Thank you for showing up for patients when it was not convenient. And thank you for the honesty many of you have brought forward in your feedback and problem-solving. Let's finish December with strong performance and take any scheduled time off seriously. Come back ready to build on what’s working and to correct what isn’t. In the new year, we will continue building a culture where quality, integrity, and trust are not just aspirational goals, but the standard we live by.
Please always feel free to reach out (Jake.Turrentine@qualderm.com) with any questions or concerns.
Sincerely,Jake E. Turrentine, MD

Clinical Corner
Scabies Misdiagnosed as Eczema: A Quiet but Widespread Blind Spot
Across the U.S. in recent years, clinicians have reported a noticeable rise in scabies masquerading as “eczema flares,” especially in primary care, urgent care, and pediatrics, and increasingly in dermatology practices. I have seen this in my own clinic, where patients referred to me after trying/failing biologics for eczema (after seeing multiple other dermatologists) were ultimately found to have undiagnosed scabies infection.
This mirrors international data showing increased transmission during and after periods of close household contact, and the clinical pattern in the U.S. is the same: generalized pruritus that peaks at night, partial steroid response with rapid relapse, lesions in finger webs or periumbilical areas, and at least one other itchy family member.
Many of these patients arrive labeled as dermatitisand have already undergone multiple rounds of steroids, antihistamines, or even biologics! The takeaway for dermatologists is clear: if a presumed eczema flare spreads despite appropriate therapy, intensifies at night, or clusters within a household - even in clean, stable homes - lower the threshold for empiric scabies treatment. And, remember to perform a simple and cost-effective test: the mineral oil prep / KOH prep to find evidence of scabies. Misclassification delays care and prolongs transmission, and this remains one of the most correctable diagnostic misses in everyday dermatologic practice.

Coding Corner
Important Changes to Skin Substitute Billing
1) Medicare spending on “skin substitutes” recently had unprecedented growth, rising from $256 million in 2019 to over $10 billion in 2024, according to Medicare Part B claims data. This dramatic spending increase was largely attributed to abusive pricing practices in the sector, including the use of products with limited evidence of clinical value. In 2025, the CMS Fraud Defense Operations Center (FDOC) stopped nearly $185 million in alleged improper payments to suspect providers billing for skin substitutes. In one notable case identified in September 2025, the FDOC stopped more than $4.3 million in suspected improper payments submitted by a medical group practice. Virtually all of the $4.3 million was for wound care services purportedly provided to a single beneficiary who lacked evidence of prior wound treatment. CMS currently treats skin substitutes as biologicals for the purposes of Medicare payment. In the CY 2026 PFS final rule, CMS will pay for skin substitutes under the PFS as incident-to supplies, a change expected to reduce Medicare spending on these products by nearly 90% without compromising patient access or quality of care.
2) What does this mean? Starting in 2026, CMS is abandoning the old ASP-based payment model for most skin substitutes and shifting nearly all non-biologic products into a single “incident-to” supply payment tied to the application procedure. Instead of each product being reimbursed according to its own price, CMS will pay a flat national rate of roughly $127 per square centimeter, regardless of whether the product is an HCT/P, 510(k) device, or PMA device. Only products with full biologics licensure will remain under the traditional ASP system (only commonly used example is Apligraf). Coding stays largely the same, but the financial foundation underneath it changes: the product becomes a supply, not a separately paid drug or biologic. The practical takeaway is that high-cost substitutes will no longer be financially sustainable under Medicare, and we will either need to be offered better pricing or shift to lower-cost options to avoid losing money. CMS has also made clear that documentation will be scrutinized more closely, especially proof of medical necessity and failure of conservative care. Providers should expect more audits and tighter claim review. I am working on additional, more detailed, separate messaging to discuss our currently available products and best practices on wound care / skin substitutes moving forward.
Compliance Updates
MIPS and CLIA
MIPS: We are doing well on MIPS measures, but there is still room for continued improvement. Quality points count as 30 percent of our total MIPS score, so our goal is to get quality scores as close to 60 points (30 percent of the total score) as possible. Here are the current standings for each of our groups within QualDerm as of mid-November.
TIN Group | Quality Points (of 60) | Percentage Score (max 30%) |
|---|---|---|
ADNCO Group | 36.52 | 18.3% |
NC Group | 40.71 | 20.3% |
Derm Affiliates | 38.89 | 19.4% |
VOO Macaione and Papa | 41.43 | 20.7% |
ZB&L Group | 42.79 | 21.4% |
Pinnacle Dermatology Group | 39.9 | 20.0% |
CSD Group | 39.02 | 19.5% |
Cumberland | 42.5 | 21.2% |
CLIA: If you are a lab director of a moderate to high complexity (non-PPM) lab, this is a final reminder to make sure to document your second site visit by the end of the year. You should have already completed your first one before September 1, and your second visit should be at least four months later. Here is our suggested template for documentation: Site Visit Template for Lab Directors.pdf.
Provider Achievements
Congratulations Gerardo Marrazzo, MD!
Dr. Gerardo Marrazzo and his wife Aubrey completed a mixed doubles HYROX competition in Chicago on November 15 with a strong performance: 1 hour, 15 minutes and 54 seconds. HYROX is a challenging race that includes eight 1000m runs, each followed by a different functional workout station, including ski ergometer, sled push, sled pull, burpee broad jumps, rowing, farmer carry, weighted lunges and wall balls.
To help us celebrate accomplishments across our network, we’ve created a link where you can report your own or a colleague’s recent achievements. Please take a moment to share by filling out the form here:
Opportunities
VisualDx Access
VisualDx Access
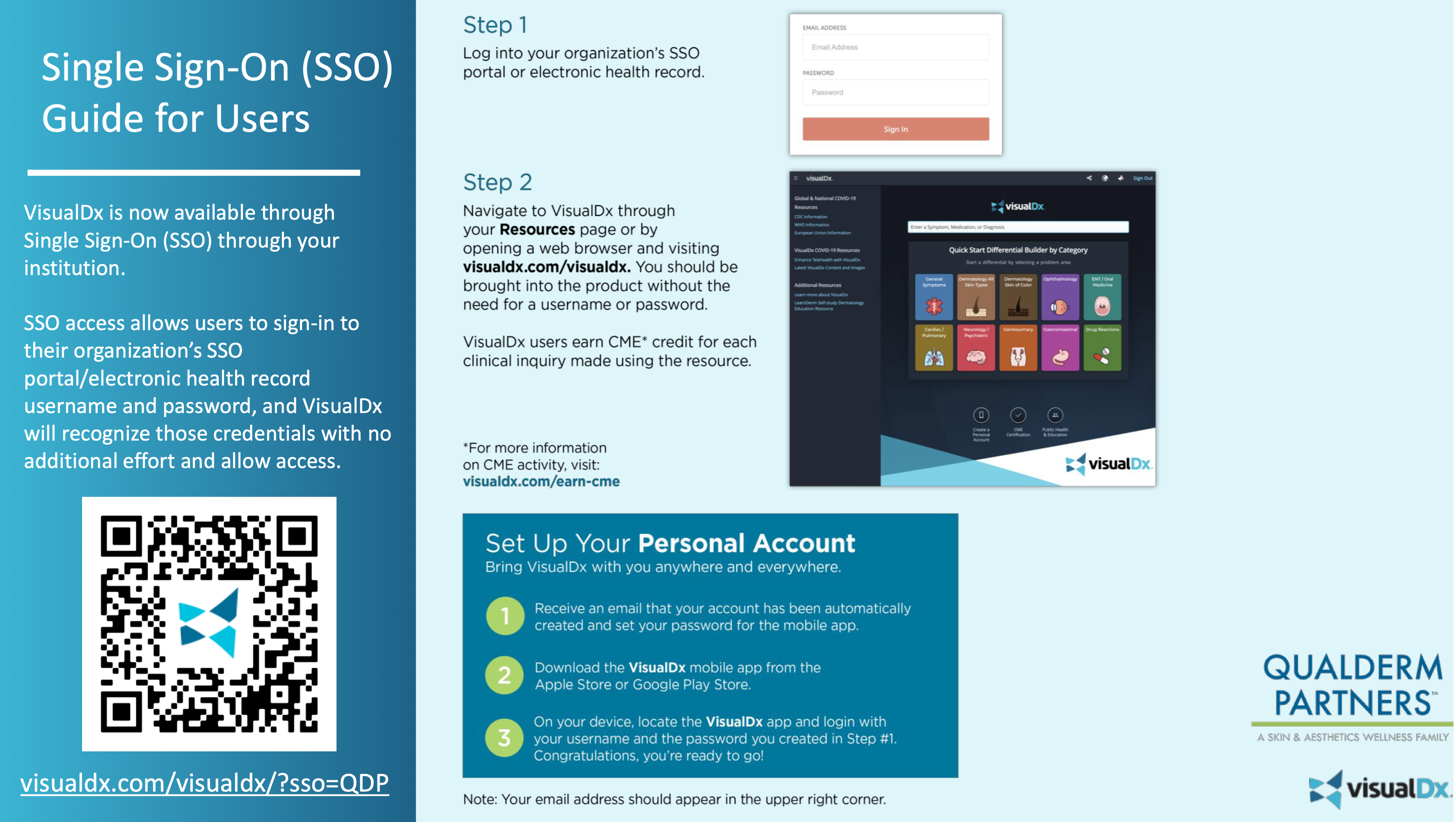
Visual Dx: All providers have paid access to VisualDx through QualDerm. This platform can assist with diagnosis and patient education. Whether you need help forming a differential diagnosis or simply want to share condition-specific information with a patient, this is an excellent resource. VisualDx even offers patient education materials in Spanish for most diagnoses! You may earn 0.5 hours of CME for each diagnosis searched, but the credit must be claimed. There are still many hours that have been earned but are still unclaimed. CME may be claimed through the VisualDx app or website.
QualDerm Helping Hand
Please help support our Helping Hand program! QualDerm Helping Hand is a teammate assistance program established to help our employees support each other. All donations are tax-deductible, and these funds are used to help qualifying teammates via Helping Hand grants. For more information about the program, and for the payroll authorization program, please click the button below. Please also feel free to reach out to Casey Parker or Marcia Topiwala with any questions.
QualDerm Advanced Therapeutics CME Conference
On Saturday, February 7, 2026, we will host our QualDerm Advanced Therapeutics CME conference from 10:00 a.m. to 4:00 p.m. EST. You will have an opportunity to earn CME credit for attending.
This will be a virtual conference covering a wide range of topics. The agenda is being finalized, but preliminary topics include:
- "Managing Itch Without Losing Your Patients (or Patience)" - Cliff Perlis
- "Cutaneous Oncology 2025 In Review: What Every Dermatologic Surgeon Should Know" - Geoffrey Lim
- "Legal Claims and Risk Mitigation in Dermatology" - Lori Chamberlain
- "Challenging Cases in Dermatopathology" - Omar Sangueza
- "Review of E/M Coding Guidelines: Documenting Properly to Get Credit for Your Work" - Jake Turrentine
We will also have lectures from speakers outside of the QDP network to discuss topics such as: psoriasis, atopic dermatitis, aesthetics, and artificial intelligence in dermatology.
The greatest danger is not that we aim too high and miss, but that we aim too low and hit. - Michelangelo

