Provider Pulse - January 2026

Welcome to 2026! We finished a strong 2025, and I appreciate all of your hard work and dedication.
Sincerely,
Jake E. Turrentine, MD

Clinical Corner
Superficial Radiation Therapy (SRT) in the Management of Non-Melanoma Skin Cancer
Non-melanoma skin cancer (NMSC), primarily basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), can be effectively treated using a range of modalities. No single approach is optimal for all tumors or all patients. Superficial radiation therapy (SRT) is a well-established, non-surgical option that plays a role in selected cases when considered alongside Mohs micrographic surgery, standard excision, electrodessication and curettage (ED&C), and topical or field therapies. Current NCCN guidelines emphasize that treatment selection should be individualized based on tumor risk factors, patient characteristics, anatomic considerations, and patient preference rather than a one-size-fits-all approach.
What is SRT?
SRT uses low-energy x-rays (typically 50–150 kVp) that penetrate only a few millimeters into tissue, delivering a cytotoxic dose to superficial tumors while sparing deeper structures. Treatment is fractionated over multiple sessions, usually across several weeks (approximately 20 treatments in most cases).
Where does SRT fit conceptually?
SRT is best understood as a local definitive treatment for appropriately selected superficial malignancies, not as a replacement for surgery in all cases. Its value lies in situations where surgical management is suboptimal due to patient factors, anatomic considerations, or patient preference after informed discussion. NCCN guidelines recognize radiation therapy as an appropriate definitive treatment option for BCC and SCC in patients who are not ideal surgical candidates or who decline surgery after informed discussion.
What are some clinical scenarios where SRT may be appropriate?
- Patients with basal cell carcinoma and squamous cell carcinoma who are poor surgical candidates due to age, anticoagulation, comorbidities, or wound-healing concerns.
- Tumors in anatomically or cosmetically sensitive areas (e.g., nasal ala, eyelids, ears) where surgery would result in functional compromise or complex reconstruction.
- Patients who decline surgery after understanding comparative cure rates, risks, and logistics.
- Selected primary BCCs or SCCs with well-defined borders and limited depth, particularly when histologic subtype and size suggest low to moderate risk.
- Recurrent disease where additional surgery would be morbid and prior pathology is well characterized.
How does SRT compare with other treatment modalities?
Mohs micrographic surgery: Mohs remains the gold standard for high-risk BCC and SCC, particularly in the head and neck, due to its high cure rates and margin control. It is preferred for aggressive histologic subtypes, recurrent tumors, tumors with poorly defined borders, and lesions at high risk for subclinical extension. SRT does not provide histologic margin assessment and is not a substitute in these settings.
Standard excision: Excision offers high cure rates for low- and intermediate-risk tumors and allows histopathologic margin evaluation. Excision is efficient, widely available, and often first-line. SRT may be considered when excision would result in unacceptable morbidity or when surgical risk outweighs benefit.
ED&C: ED&C is effective for appropriately selected low-risk BCCs and SCC in situ in non-cosmetically sensitive sites. It is quick and cost-effective but operator-dependent and limited by lack of margin control. SRT may be preferable when cosmetic outcome, lesion location, or tumor depth make ED&C less suitable.
Topical and field therapies (e.g., 5-FU, imiquimod, PDT): Topical therapies are primarily used for superficial BCC, SCC in situ, and field cancerization. They have lower cure rates than surgery or radiation and rely heavily on patient adherence. SRT offers a non-topical, provider-controlled alternative when topical therapy fails, is contraindicated, or is declined.
Limitations and risks of SRT:
- Requires multiple visits over weeks, which may be burdensome for some patients.
- Does not provide histologic margin confirmation. However, image guided SRT (IG-SRT) may help improve confirmation of tumor clearance, though it is not histologic margin confirmation.
- Late effects can include hypopigmentation, telangiectasia, skin atrophy, or fibrosis.
- Radiation exposure precludes repeat treatment at the same site and may complicate future surgical management.
- Sometimes avoided in younger patients due to long-term theoretical risks and better surgical alternatives.
Bottom Line – SRT should be considered as one of many modalities to treat NMSC, and treatment decisions should be based on patients’ informed decision making: The choice of therapy for NMSC should be individualized, incorporating tumor risk factors, patient comorbidities, life expectancy, cosmetic and functional priorities, and patient values. SRT should be presented as one option among several - not as superior to other options, but as a reasonable choice in appropriate clinical contexts.
Coding Corner
Important Changes to Skin Substitute Billing
As we start the new year, I would like to review for all our providers the key points of the Medical Decision Making Table (MDM table), which determines your coding level in 2026:
https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf
Over the last several years, confusion around E/M coding has not come from lack of effort, but from a mismatch between how dermatologists practice and how the MDM table is actually applied in audit. This month, in addition to clarifying the overall framework, I’d like to point to a common point of misunderstanding: what does, and does not, count as prescription drug management?
The MDM table has three elements: (1) problems addressed, (2) data reviewed/analyzed, and (3) risk of complications and/or morbidity or mortality of management. The overall MDM level is the highest level where two of the three elements are met.
Psoriasis provides a clean example. When psoriasis is stable and the visit consists of confirming control and continuing the existing plan, the problem element is low (stable chronic illness). The data reviewed is usually none (straightforward). The risk element is also low unless the documentation shows active prescription decision-making. In that scenario, the visit is low MDM, even though the medication itself is significant. Even if the risk element was moderate or high, the highest level where 2/3 elements are met would still be low, because a single stable chronic illness is a low-complexity problem.
A visit reaches moderate MDM (mapping to 99214) when two elements rise together. In dermatology, the most common and defensible pathway is moderate problem plus moderate risk. Using psoriasis again: when the disease is flaring, not at goal, or failing prior therapy, the problem element is moderate. If that instability leads to starting, stopping, switching, or escalating prescription therapy, or to an explicitly documented decision to continue a medication after reassessment, the risk element is also moderate. At that point, the visit meets two moderate elements regardless of data. Alternatively, moderate problem plus moderate data (e.g., meaningful of outside records that inform management and/or ordering of enough relevant labs) can also support moderate MDM.
The practical takeaway is this: the MDM table rewards documented decision-making, not diagnoses, medication names, or note length. Stable disease plus passive continuation is low MDM. Disease instability that forces a treatment decision is moderate MDM. Active prescription management, including a reasoned decision to continue therapy, must be visible in the record to be credited. When providers understand and document along these lines, coding becomes both accurate and defensible, without changing how good dermatology is practiced.
Compliance Updates
MIPS and CLIA
- MIPS: We closed 2025 with record MIPS Quality Scores, exceeding 20 percent of the maximum possible 30 percent for the Quality category for all our practices. I am proud of our providers company-wide for doing so well. Later this month, we will confirm the quality measures that we will be tracking for 2026. At this point, my understanding is that we will be tracking the same quality measures that we tracked for 2025, unless we can identify stronger measures that are more relevant to our practices. Given that we now understand these measures, we have an opportunity to do even better on our MIPS Quality Scores in 2026. It is important to understand that as everyone around the country performs better, the threshold to achieve high scores becomes more difficult to achieve. Therefore, it is best to start at the very beginning of the year with a focus on achieving 100 percent accuracy, rather than playing “catch up” later in the year. As a reminder, these are the measures we are tracking:
- 47: Advance Care Plan: The percentage of patients aged 65 years or older who have an Advance Care Plan or surrogate decision maker documented in the medical record.
- 226: Tobacco use screening & cessation intervention: This is a two-part measure. The first is screening (if non-smoker, or former smoker, then you are done and the visit is favorable). The second is cessation intervention (if the patient admits to smoking, then counseling must be provided and documented in MIPS).
- 238: High risk meds in older adults: This is an automated measure based on your prescribing practices. It measures the percentage of patients 65 years of age and older who were ordered at least two high-risk medications from the same drug class. You want the percentage to be zero, so providers should avoid prescribing two high risk medications from the same class.
- 394: Immunizations in Adolescents: For patients who were 12 at any point in 2026 (recently turned 13 but were 12 at the start of the year, are 12 at the time of the visit, or are 11 and about to turn 12), then you must document their vaccine status for Tdap, Meningococcal and HPV vaccine. You get credit if they have gotten all 3 vaccines. If they have an upcoming pediatric appointment for their vaccines, put a reminder to get their vaccine records and update the MIPS after their pediatrician visit.
- 485: Improvement in Psoriasis Itch Severity: This measure requires a diagnosis of psoriasis, two (2) qualifying encounter codes and the numeric itch rating for patients 18 and older. There must be an itch score of 4 or more on the first visit and must decrease by 3 or more points on the second visit for this to be “favorable”. If the itch score is 3 or less at the first psoriasis visit, then that visit will not count towards the measure. However, if there is a previous visit where the score was 4 or more, then the visit where the score is 3 or less will count as a follow-up visit, and favorability will be based on whether the score dropped by 3 or more points.
- 486: Improvement in Dermatitis Itch Severity: This measure requires a diagnosis of Dermatitis, two (2) qualifying encounter codes and the Numeric Itch Rating for patients 18 and older. ** There must be an itch score of 4 or more on the first visit, and it must decrease by 3 or more points on the second visit for this to be favorable.• Atopic Dermatitis (L20.89)
- Irritant Contact Dermatitis (L24.XX)
- Allergic Contact Dermatitis (L23.XX)
- Nummular Dermatitis (L30.0)
- Dermatitis Unspecified (L30.9)
- 410: Clinical Response to Systemic Medications: A patient with known psoriasis with systemic or biologic medication listed in their “Clipboard” will qualify for this measure. A psoriasis patient with a systemic or biologic ordered in the “Virtual Exam Room” will qualify for this measure. If patients are NOT at treatment goal, then it is critical to select an EXCEPTION to earn appropriate MIPS credit. This is probably the single biggest area where we can improve as a company on our MIPS documentation.
- 355: Unplanned reoperation within the 30 day post operative period: This measure is related to complications from soft tissue excision procedures and only qualifies with certain soft tissue excision codes (e.g. lipomas). The goal is to demonstrate that we have low rates of complications from these types of procedures (e.g. complications such as hematomas that require re-operation). It only applies in the 30 days following a qualifying soft tissue excision procedure.
- 357: Surgical site infection (SSI): This measure is also related to complications from soft tissue excision procedures and only qualifies with certain soft tissue excision codes (e.g. lipomas). The goal is to demonstrate that we have low post-operative infection rates. It only applies in the 30 days following a qualifying soft tissue excision procedure and is captured automatically.
- 509: Melanoma Tracking / Recurrence: This measure has 3 parts. The first question is the “denominator” question where you confirm that the patient had a stage 0, I, or II melanoma surgically removed in the last 5 years. The second question is whether or not the patient had an exam to evaluate recurrence of the melanoma, and the third question is whether or not they have had a recurrence. To achieve a favorable score, patients who have had a melanoma in the last 5 years should have an exam to evaluate for recurrence and there should be no recurrence.
Provider Achievements
We are actively collecting provider achievements to celebrate each other this year. Please bookmark this link and use it often to recognize your peer. Let’s celebrate publications, athletic achievements, committee appointments, awards won, or anything else you think deserves a shout out!
Opportunities
QualDerm Advanced Therapeutics CME Conference
On Saturday, February 7, 2026, we will host our QualDerm Advanced Therapeutics CME conference from 10:00 a.m. to 4:00 p.m. EST. You will have an opportunity to earn CME credit for attending.
This will be a virtual conference covering a wide range of topics. The agenda is being finalized, but preliminary topics include:
- "Managing Itch Without Losing Your Patients (or Patience)" - Cliff Perlis
- "Cutaneous Oncology 2025 In Review: What Every Dermatologic Surgeon Should Know" - Geoffrey Lim
- "Legal Claims and Risk Mitigation in Dermatology" - Lori Chamberlain
- "Challenging Cases in Dermatopathology" - Omar Sangueza
- "Review of E/M Coding Guidelines: Documenting Properly to Get Credit for Your Work" - Jake Turrentine
We will also have lectures from speakers outside of the QDP network to discuss topics such as: psoriasis, atopic dermatitis, aesthetics, and artificial intelligence in dermatology.
VisualDx Access
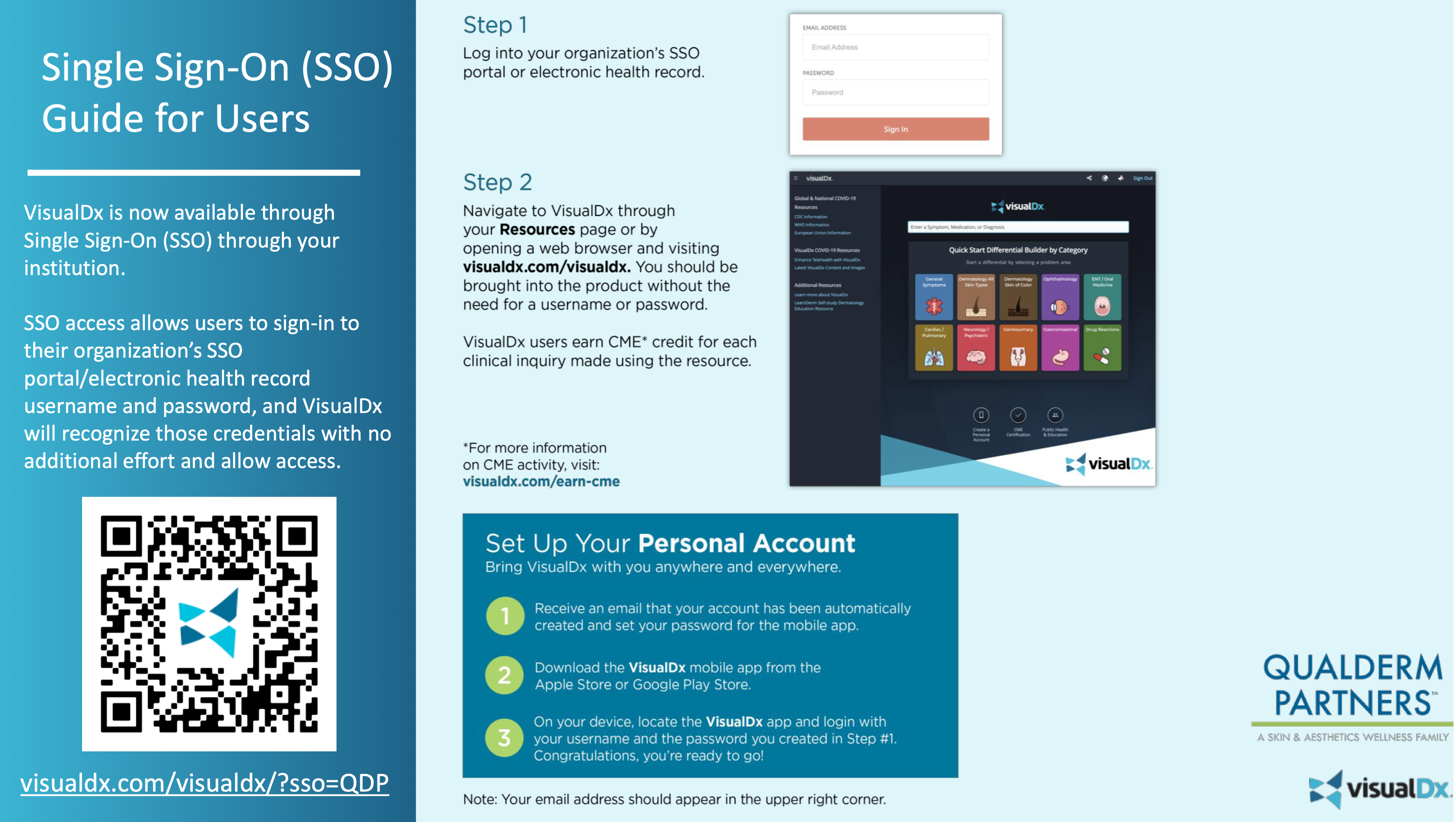
VisualDx Access
Visual Dx: All providers have paid access to VisualDx through QualDerm. This platform can assist with diagnosis and patient education. Whether you need help forming a differential diagnosis or simply want to share condition-specific information with a patient, this is an excellent resource. VisualDx even offers patient education materials in Spanish for most diagnoses! You may earn 0.5 hours of CME for each diagnosis searched, but the credit must be claimed. There are still many hours that have been earned but are still unclaimed. CME may be claimed through the VisualDx app or website.
QualDerm Helping Hand
Please help support our Helping Hand program! QualDerm Helping Hand is a teammate assistance program established to help our employees support each other. All donations are tax-deductible, and these funds are used to help qualifying teammates via Helping Hand grants. For more information about the program, and for the payroll authorization program, please click the button below. Please also feel free to reach out to Casey Parker or Marcia Topiwala with any questions.
The beginning is the most important part of the work. - Plato

