Provider Pulse - October 2025
 Dear Colleagues:
Dear Colleagues:As we turn the corner into the final stretch of 2025, I want to thank you for the commitment you’ve shown to your patients, your teams, and QualDerm as a whole. Our collective work this year has been extraordinary. We’ve steadily strengthened clinic performance, improved patient experience metrics across multiple regions, and brought new providers into the fold who are already thriving because of your mentorship and collaboration.
This is the time of year when discipline matters most. The finish line may be in sight, but how we show up in these last months will define our trajectory into 2026. Every clinic day, every patient encounter, and every quality decision you make moves us closer to our shared goal: to be the standard for excellence in dermatology care and skin health.
A quick reminder as we enter this home stretch: please ensure that MIPS measures are addressed at each visit where they are applicable. Each completed measure directly impacts our organizational score and future reimbursement. Please also make sure documentation is thorough and quality metrics are captured. Although this may feel like a regulatory exercise, MIPS is currently our best objective method to demonstrate the quality of the care you deliver every day.
Thank you for the hard work, the teamwork, and the heart you bring to this organization. I’m proud to serve alongside you, and I’m always here to help tackle issues that arise. Let’s finish the year strong and set the stage for an even bigger leap forward in 2026.
Please always feel free to reach out (Jake.Turrentine@qualderm.com) with any questions or concerns.
Sincerely,Jake E. Turrentine, MD

Clinical Corner
Staying Prepared for Aesthetic Procedure Complications
As demand for aesthetic procedures continues to surge, so does the responsibility to be fully prepared for the rare but serious complications that can occur. A recent Dermatology World feature highlighted that while dermatologists strive to keep patients safe, complications are “bound to occur in some form or fashion,” particularly in the high-volume, high-efficiency world of cosmetic dermatology.
Severe events, though uncommon, can be devastating if not recognized and treated immediately. These include:
- Allergic reactions (including anaphylaxis)
- Vascular compromise or embolism (e.g., filler-related)
- Vision loss or blindness
- Tissue necrosis or disfigurement
Providers performing or supervising procedures such as botulinum toxin injections, dermal fillers, and other minimally invasive aesthetics must be confident in recognizing warning signs and have rapid access to appropriate countermeasures. This includes familiarity with the use and location of reversal agents such as hyaluronidase, as well as epinephrine, aspirin, nitroglycerin paste, and warm compress/massage protocols when indicated.
Being prepared—clinically, mentally, and logistically—is our best defense for patient safety and for our own medicolegal protection. In the words of one colleague: “People will line up to testify against you… unless you are ready to do the right thing, fast.”
Complications may be rare, but they are high-stakes. These include vascular occlusion, embolism, vision loss, tissue necrosis, anaphylaxis, or severe infection. The difference between full recovery and permanent injury often comes down to seconds and minutes, not hours.

Practical Steps for Providers
1. Know the Warning Signs
Ensure all injectors and support staff can quickly recognize early signs of:
- Vascular compromise: blanching, dusky discoloration, livedo, and/or severe pain out of proportion to injection
- Impending blindness: acute visual changes, ocular pain, and/or headache during or immediately after injection
- Allergic/anaphylactic reactions: urticaria, wheezing, swelling, and/or hypotension
- Infection: delayed swelling, erythema, and/or tenderness beyond the expected course
2. Maintain Immediate Access to Emergency Medications
Every location where injectables are performed should have a readily accessible, organized aesthetic emergency kit that includes, at minimum:
- Hyaluronidase (multiple vials, not expired, with instructions for reconstitution and injection grid dosing)
- Aspirin (325 mg) and nitroglycerin paste for vascular compromise
- Epinephrine autoinjector (0.3 mg) and oral antihistamines/corticosteroids for anaphylaxis
- Warm compresses and massage tools for early filler vascular events
- Topical and oral antibiotics (as indicated)
All providers must know where this kit is stored and how to use it. Assign responsibility for monthly inventory and expiration checks.
3. Establish a Rapid Response Workflow
Time matters. Have a clear plan for:
- Who is called first (on-site physician supervisor, back-up aesthetic physician, or another designated provider)
- Where to send the patient if escalation is needed (local ED, oculoplastics, vascular surgery, urgent care)
- Documentation and reporting (photographs, note template, informed consent copy)
4. Maintain Competency Through Education
- Routine hands-on training or CME covering complication recognition and management
- Team debriefs after complications to reinforce learning and strengthen system response
5. Legal & Risk Considerations
Use comprehensive informed consent that explicitly covers rare but serious complications
Document lot numbers, injection sites, and immediate post-procedure assessments
Ensure all injectors are credentialed, trained, and practicing within scope
Coding Corner
Appropriate Coding of Soft Tissue Excisions
This month’s topic is the appropriate coding of soft tissue excisions. The Current Procedural Terminology (CPT) manual includes codes for reporting the excision of soft tissue lesions (such as lipomas or angiolipomas) in the musculoskeletal section. The key distinction between codes used for excision of lesions located in the integumentary section versus the musculoskeletal section is the origin of the lesion or tumor.
Excision of lesions of cutaneous origin (e.g., nevus, dermatofibroma, cyst, or carcinoma) is reported with CPT codes 11400–11646. Code selection is based on anatomic location and the size of the lesion plus the margins required for complete excision. Documentation must specify that the excision was “full thickness” (i.e., through the dermis). Excision of cutaneous lesions includes simple closure; intermediate or complex closures, when performed, are reported in addition to the excision.
CPT Codes Overview
CPT Codes | CPT Section | Lesion Type | Repair Included in Code | Office Setting (POS 11) Considerations |
|---|---|---|---|---|
11400–11646 | Integumentary | Cutaneous growth (e.g., nevus, cyst, cancer) | Simple (intermediate or complex reported separately) | Almost always covered |
| 21011–28039 | Musculoskeletal | Subcutaneous growth (e.g., lipoma, angiolipoma) | Simple or intermediate (complex reported separately) | Certain codes considered “rarely or never” performed in the office setting |
In contrast, excision of tumors of subcutaneous origin (e.g., lipomas/angiolipomas) is reported with CPT codes from the musculoskeletal section. Code selection depends on the anatomic location, the depth of the lipoma (subcutaneous vs. subfascial), and the size of the lesion. Size is determined by the greatest diameter of the lipoma plus the margin required for complete excision.
Excision of lipomas or other soft tissue tumors includes simple or intermediate repairs. Complex repairs requiring extensive undermining or other techniques should be reported separately. Dissection or elevation of tissue planes to allow for resection of the lipoma is included in the excision and not separately reportable.
Documentation in ModMed/EMA
When documenting lipoma excision in ModMed/EMA, use the Soft Tissue Excision plan. Enter:
- the body location
- the excised diameter
- the excised depth
- the excision type
EMA will then generate the correct soft tissue excision code.
If a complex repair is performed after lipoma excision and is supported by documentation, note that EMA will not automatically add the code for the repair due to NCCI coding edits. In this case, use the Repair Note plan to generate the repair code or override billing and add the appropriate code manually, appending modifier -59.
Coverage and Reimbursement Considerations
Certain lipoma excisions are considered by CMS to be “rarely or never performed” in an office setting. Depending on the location, anatomic site, and depth of excision, procedures may be denied or reimbursed at a reduced rate. Private and commercial payers often have separate payment policies, although Medicare guidelines generally provide the foundation. Some insurers may deny coverage for office-based soft tissue excisions regardless of CMS allowances.
A general rule:
- Subcutaneous (not subfascial) lipomas < 3 cm are almost always covered in the office, except on the face or scalp, where the size must be < 2 cm.
- Some payers do reimburse larger or deeper lipomas in-office, but CMS designates most of these as “rarely or never” performed in this setting, making reimbursement less likely.
- For larger or subfascial lipomas, prior authorization is recommended.
Full guidance on soft tissue excision codes is provided in the Compass Coding Consultants handout.
Provider Achievements
Congratulations Megan Rahn!
Megan Rahn, NP, was highlighted in the Weekly View community newspaper for quickly arranging evaluation of a patient’s lesion that was diagnosed as melanoma and for rapidly coordinating the patient’s care.
To help us celebrate accomplishments across our network, we’ve created a link where you can report your own or a colleague’s recent achievements. Please take a moment to share by filling out the form here:
Opportunities
VisualDx Access
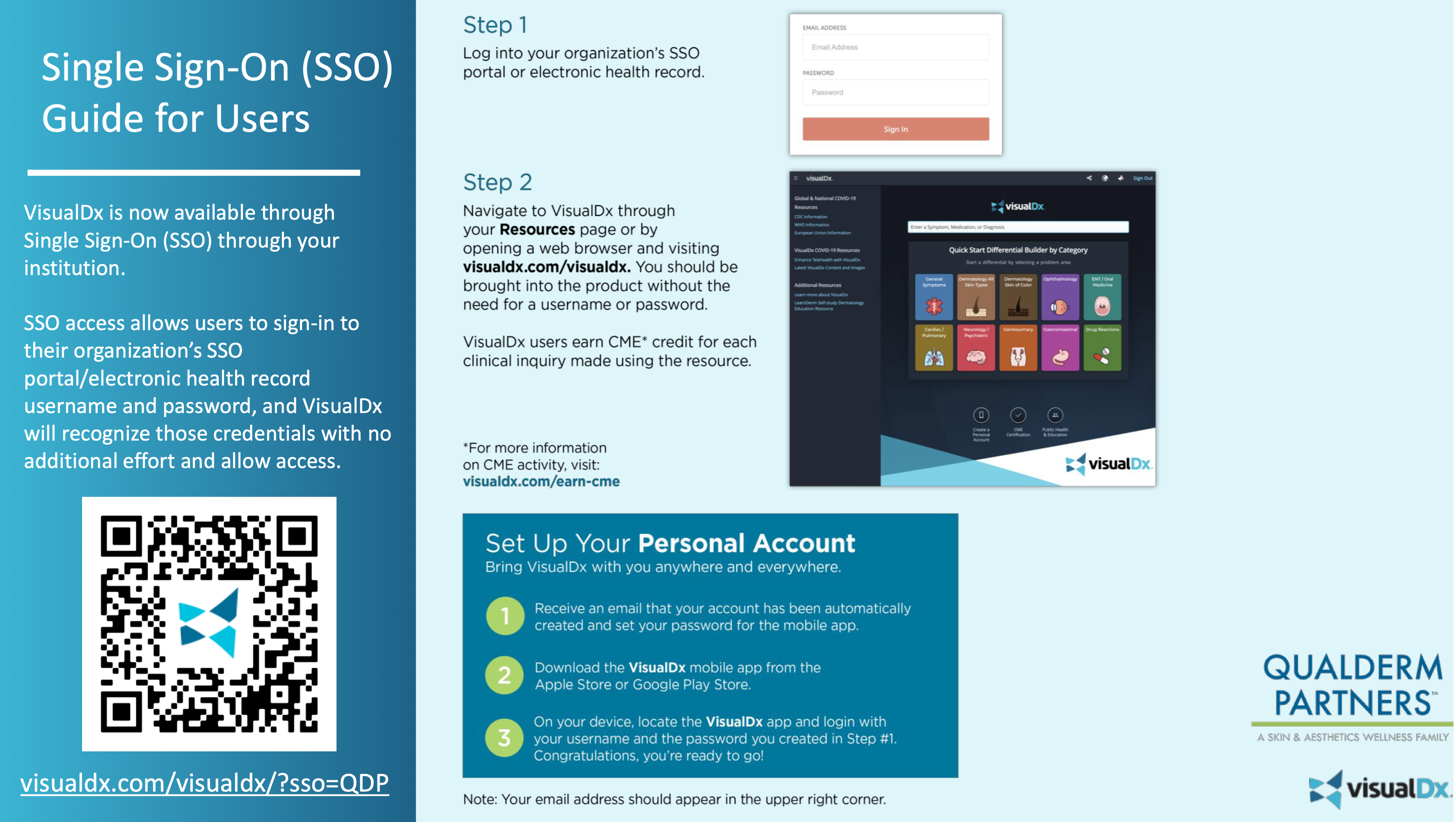
All providers have paid access to VisualDx through QualDerm. This platform is an excellent tool to support diagnosis and patient education. Whether you need help forming a differential diagnosis or want to share condition-specific information with a patient, VisualDx can assist. Patient education materials are even available in Spanish for most diagnoses. We recently learned that providers may earn 0.5 hours of CME for each diagnosis searched—but the credit must be claimed. Only about 4.4% of eligible CME hours were claimed in the past year. Based on unclaimed searches, that represents roughly 8,000 hours of CME earned but not claimed across QualDerm. CME credit can be claimed through the VisualDx app or website.
Grand Rounds
Grand Rounds is an excellent opportunity for us to collaborate, share great cases, and earn CME credit. We recently learned that presenters may earn up to 1 additional hour of CME credit for every 15 minutes of presentation time (in addition to the full hour granted for participating in Grand Rounds). If you prepare a single case to present, up to 1 hour of preparation time can count toward credit. Our next Grand Rounds is November 4, 2025, at 8:00 p.m. EST. CME credit is offered if 4–5 cases are submitted in advance of the meeting. Please continue to watch for strong cases that would benefit our provider network. If you have a case to share, please reply to Sheri Kimbro with your topic; she will assist with the logistics for your presentation. As a thank-you, presenters will receive QDP swag—such as coffee mugs, tumblers, or tote bags.
QualDerm Helping Hand
Please help support our Helping Hand program! QualDerm Helping Hand is a teammate assistance program established to help employees support one another. Since its inception in late 2020, Helping Hand has assisted 145 teammates with cumulative grants totaling nearly $145,000. Assistance has covered funeral expenses, family crises, caregiving needs, and unexpected income loss within teammate families. The program is completely funded by teammates, for teammates. It’s simple to participate: you may make a one-time donation or designate $1.00 or more to be automatically contributed from your biweekly paycheck. All donations are tax-deductible and fund Helping Hand grants for qualifying teammates. For more information about the program, and for the payroll authorization program, please click the button below. Please also feel free to reach out to Casey Parker or Marcia Topiwala with any questions.
The difference between ordinary and extraordinary is that little extra. — Jimmy Johnson


