An update from our Chief Medical Officer:
A lot has transpired in the last two weeks since my last update. The COVID-19 situation continues to evolve rapidly, in some ways both predictable and not. Undoubtedly and thankfully, our collective mitigation efforts have flattened the national curve and a recent study concludes that the strict lockdown measures may have prevented 60 million US infections and with a case fatality rate of 0.4 per million, saved possibly 240,000 American lives. Unfortunately, the economic impact and toll on other health conditions, both physical and mental, has been dramatic. Now with a focus on a ‘Reopening’ of our lives, very possibly prematurely in some areas, we need to navigate our new normal with the best evidence to ensure positive health outcomes and reduce the risk of surges in infection. Ongoing protests and civil unrest also complicate the balance between political action and ensuring public safety. As I mention each time in these updates, WE CANNOT LET OUR GUARD DOWN. All safety measures from our Reopening Checklist will remain in place for an undefined period of time. The reasons for this will become quite clear when reading below.
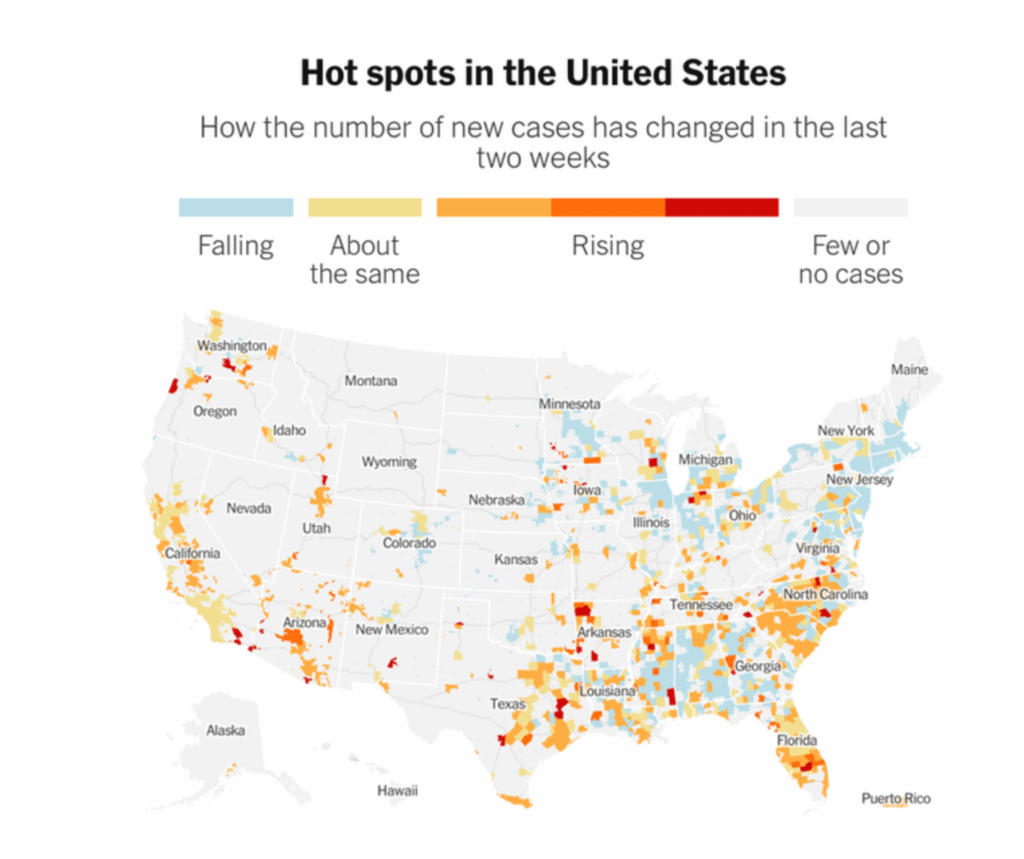
Several weeks after US states began to relax social distancing measures and “stay at home” orders as well as celebrations over the Memorial Day holiday weekend, a number of states are reporting increasing COVID-19 incidence. Analysis published by NPR identifies 23 US states with increasing COVID-19 incidence over the past 2 weeks, including 5 states with more than double the daily incidence compared to 2 weeks ago. Indeed, daily new infections are at their highest level ever in many places, including California, Florida, and Texas — the three most populous states in the country, where over a quarter of Americans live. It’s important to also realize that there is a considerable time lag between infection and showing symptoms, typically between a few days and two weeks. That means these surges in infection are so far mostly due to things that happened before the recent explosion of protests. There might be considerably sharper spikes over the next week or so.
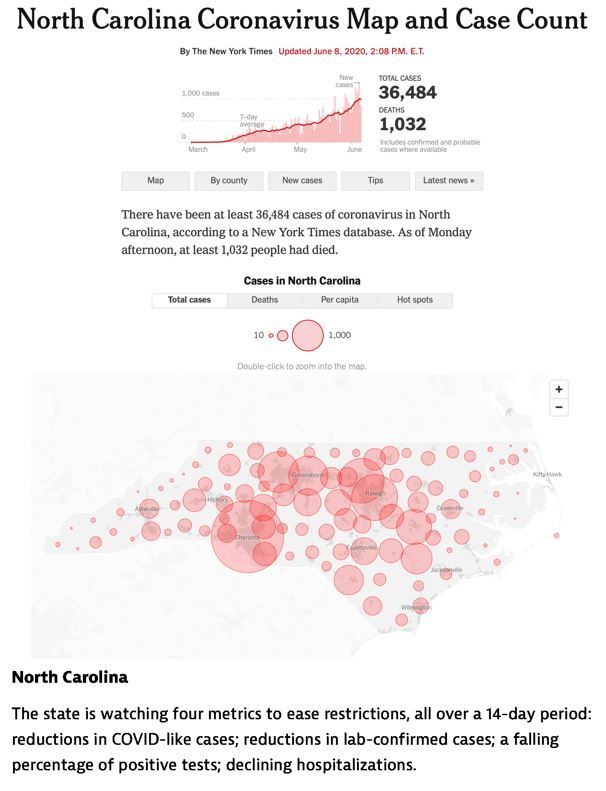
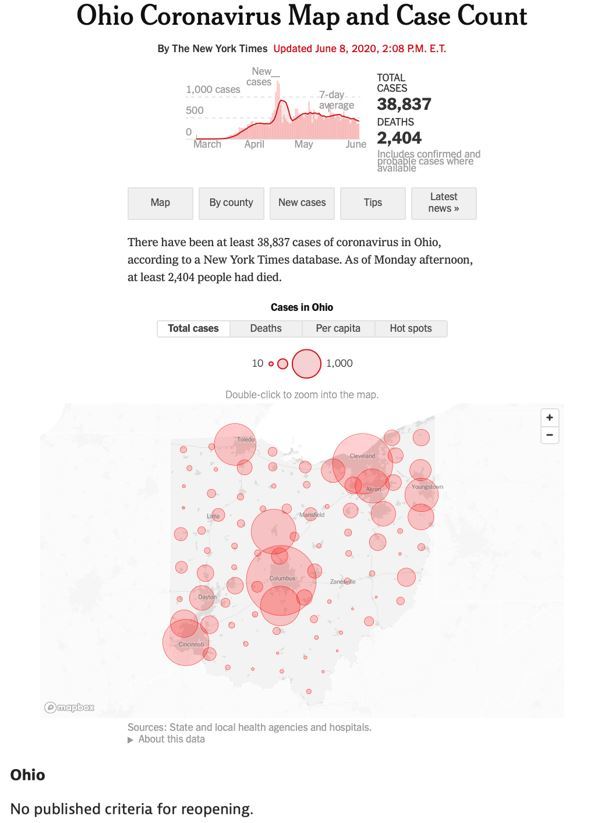
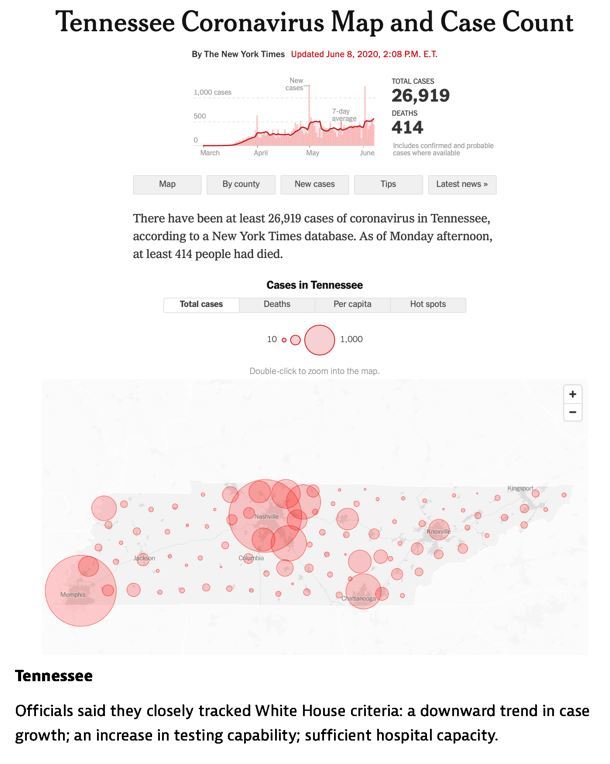
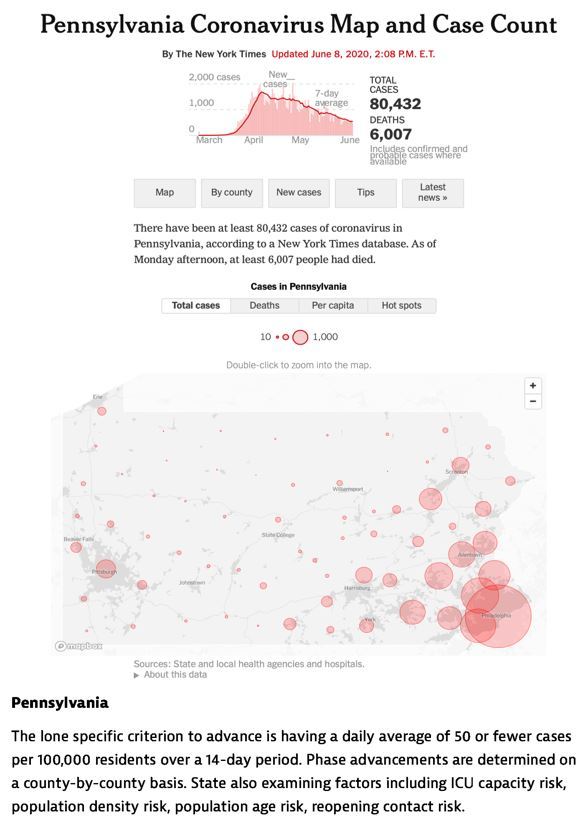
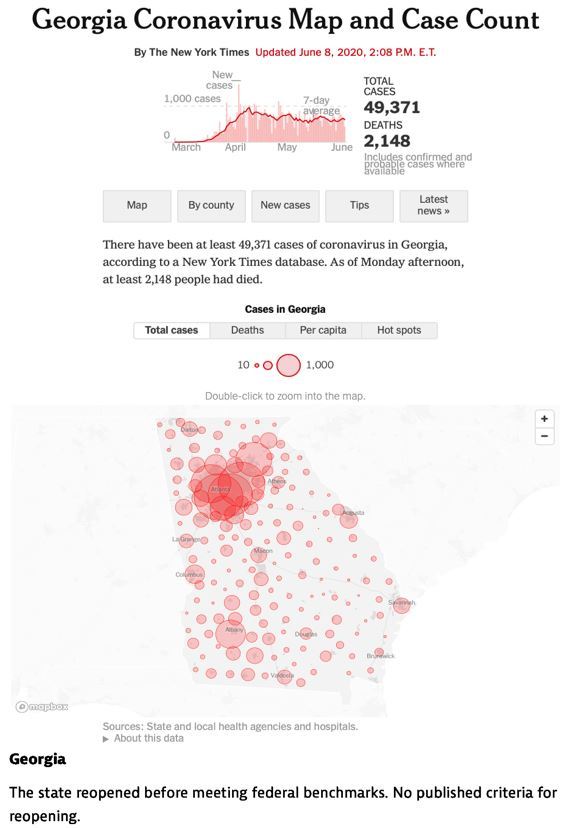
In QualDerm markets, NC, SC and TN remain on the upswing in infections and hospitalizations, a better indicator of intensity, because if rising numbers were only due to increased testing, then the percentile of positives would fall along with fewer severe cases. The opposite is happening in many places as indicated below.
We do not have a national test, trace, and isolate system, one that requires at least 100,000 contact tracers according to available data. Therefore, personal behavior is now the last line of defense against the coronavirus. Wash your hands, stay home if sick, wear a mask, maintain social distancing, and prioritize outdoor activity and congregation. At work, assume everyone is potentially infectious, utilize appropriate PPE and universal precautions.
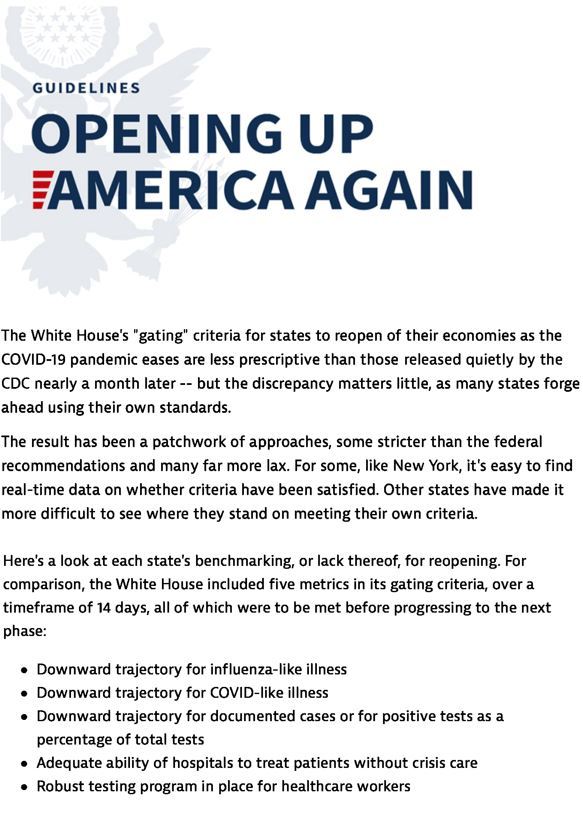
Variable State Reopening Plans have been inconsistent with CDC “Reopening America” Gating Criteria
Asymptomatic Transmission
Many of you may have read confusing statements about asymptomatic transmission risks and I wanted to provide further clarification from WHO.
At the June 8 COVID-19 media briefing, Dr. Maria Van Kerkhove, Technical Lead for the WHO COVID-19 response, commented in response to a journalist’s question that current evidence suggests that asymptomatic transmission is possible but “very rare,” based on data from available studies. The comment garnered significant attention, including uncertainty about how to interpret the statement in the context of the ongoing pandemic response, which prompted the WHO to clarify the statement to provide additional detail and put the statement in the proper context.
“The WHO created confusion yesterday when it reported that asymptomatic patients rarely spread the disease,” an email from the Harvard Global Health Institute said Tuesday. “All of the best evidence suggests that people without symptoms can and do readily spread SARS-CoV-2, the virus that causes Covid-19. In fact, some evidence suggests that people may be most infectious in the days before they become symptomatic — that is, in the presymptomatic phase when they feel well, have no symptoms, but may be shedding substantial amounts of virus.”
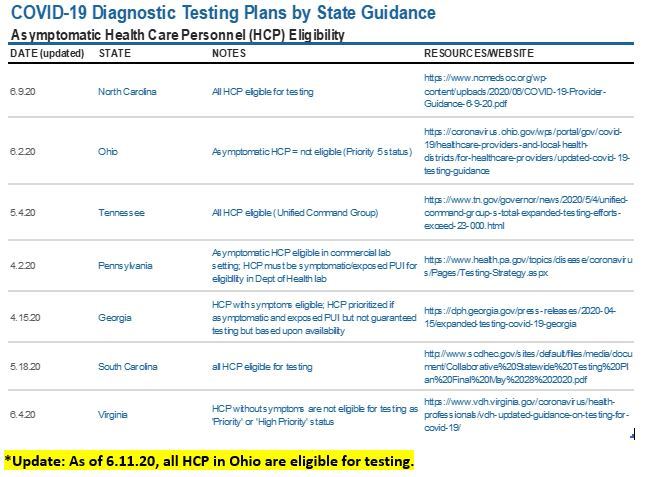
Testing
Many of you have appropriately been inquiring about testing strategies for our practices, patients and personnel, which have been delegated to individual states in an uncoordinated manner. I compiled all the guidance and orders from each QDP market below to help provide recommendations for Health Care Personnel along with links. This is NOT antibody testing, which remains unreliable for individuals.
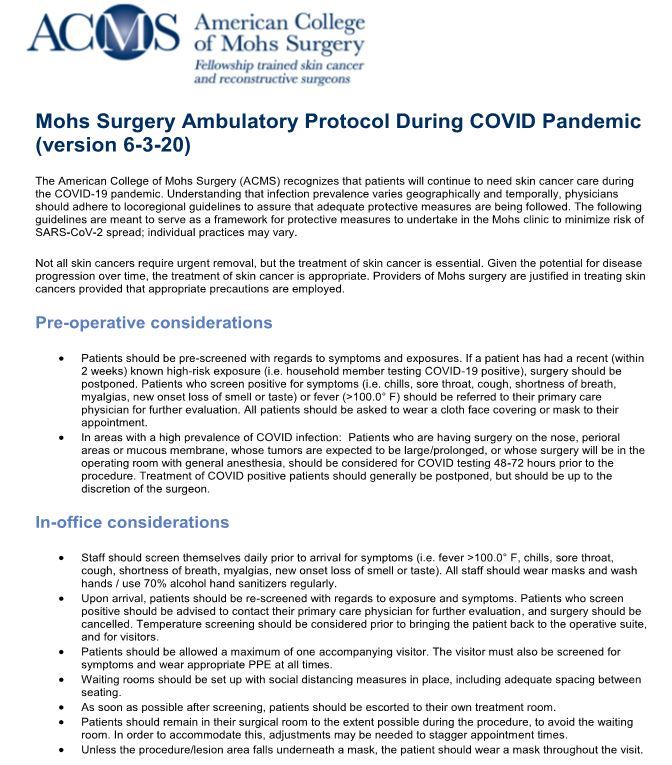
The American College of Mohs Surgery tasked the Scientific Advisory Committee, of which I am a member, with development of a Mohs Surgery Ambulatory Protocol During COVID Pandemic. As these collaborative guidelines were established with colleagues from major academic centers, I was gratified that our Quality Council endorsed QualDerm recommendations were entirely consistent and already implemented months ago. I include this guidance below for reference by all Mohs practices.
I conclude once again with a plea to continue taking care of yourselves, your patients, and your teammates. Be kind, assume good intent, and stay safe. The fatigue and stress of this crisis is undeniable and requires us all to lean on each other and recognize when we need some assistance. We all remain grateful for your dedication to our mission and I am proud of you all and our dermatology company, the best in the business.
Sincerely,
John Albertini, MD